Celiac disease and pregnancy are two conditions that require special attention when they overlap.
However, modern medical research and nutritional science confirm that with proper management, women with Celiac disease can expect outcomes comparable to the general population.
For women who are pregnant or planning to conceive, managing this condition is crucial for both maternal health and the baby’s development.
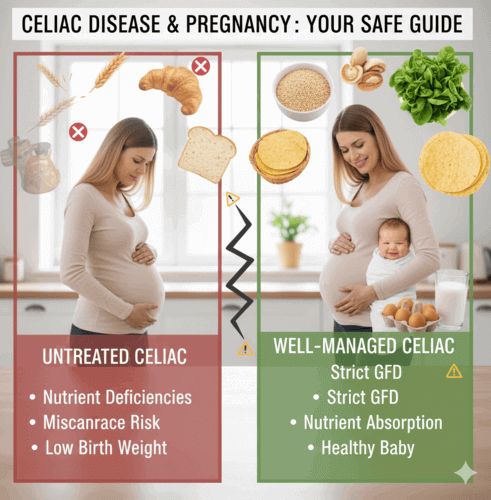
Without proper care, untreated celiac disease during pregnancy can lead to complications such as nutrient deficiencies, miscarriage, or low birth weight.
Fortunately, with early diagnosis, a strict gluten-free diet, and regular medical follow-up, most women with celiac disease can enjoy a healthy pregnancy and deliver healthy babies.
What is Celiac Disease?
Celiac disease is a lifelong autoimmune disorder where gluten intake causes the immune system to attack the small intestine. Iron, folate, calcium, and other vital nutrients, all of which are particularly crucial during pregnancy, are less readily absorbed as a result of this damage.
Because nutrition plays a critical role in fetal development, the connection between celiac disease and pregnancy must not be overlooked.
How Celiac Disease Affects Pregnancy
Fertility Challenges
One reason why celiac disease and pregnancy are often discussed together is the impact on fertility. Women with undiagnosed celiac disease may experience irregular cycles or unexplained infertility.
Once treated with a gluten-free diet, fertility rates improve.
Risks During Pregnancy
Pregnancy outcomes may be affected if celiac disease is unmanaged. Potential risks include:
- Miscarriage
- Preterm birth
- Low birth weight
- Stillbirth in severe cases
By strictly managing celiac disease before and during pregnancy, these risks can be greatly reduced.
Nutrient Deficiencies
Celiac disease limits nutrient absorption, increasing the risk of anemia, vitamin D deficiency, and low calcium levels. This can have an impact on both maternal and fetal health while pregnant.
Impact on Baby
The link between celiac disease and pregnancy is important for the baby’s development. Poor maternal nutrition may lead to intrauterine growth restriction (IUGR), low birth weight, or developmental challenges. A strict gluten-free diet lowers these risks.
Symptoms of Celiac Disease During Pregnancy
Symptoms of celiac disease often overlap with pregnancy discomforts, making it harder to diagnose. Women may notice:
- Digestive issues: bloating, diarrhea, constipation, or abdominal pain
- Non-digestive issues: fatigue, anemia, or itchy rash
- Delayed fetal growth due to malnutrition
Because these symptoms may mimic pregnancy-related changes, testing is essential when concerns arise.
Diagnosing Celiac Disease in Pregnancy
When dealing with celiac disease and pregnancy, early diagnosis is key. Doctors may recommend:
- Blood tests to detect antibodies such as tTG-IgA.
- Biopsy (sometimes postponed until after delivery).
- Symptom review and medical history assessment.
Timely testing ensures better care for both mother and baby.
Pre-Conception Planning is Key
The success of managing Celiac during pregnancy largely depends on the preparation done before conception. Think of this phase as building a strong nutritional foundation for nine months of rapid growth and change.
Establishing Celiac Remission
The absolute priority is ensuring your Celiac disease is in a state of remission. Uncontrolled celiac symptoms, which indicate active inflammation and intestinal damage, can interfere with the absorption of critical nutrients.
Active inflammation may potentially increase risks for both the mother and the developing fetus. You should be symptom-free, and ideally, your gastroenterologist should confirm remission through blood tests that measure Celiac antibodies (like tTG-IgA).
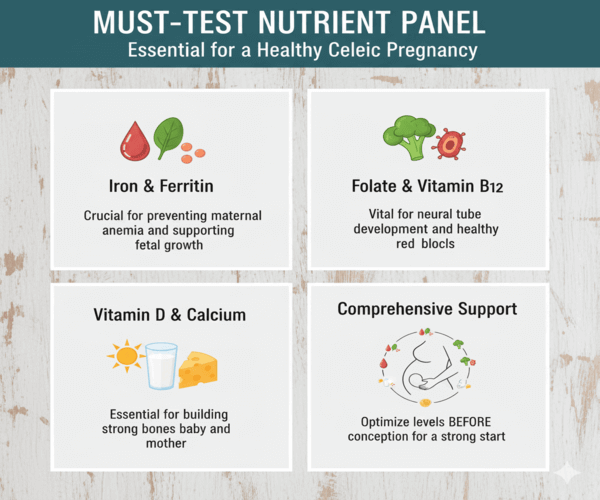
The “Must-Test” Nutrient Panel
Because of chronic malabsorption, many women with celiac disease and pregnancy concerns begin their journey with low nutrient reserves. Before trying to conceive, it’s important to work with your healthcare provider to test and optimize these essential levels:
- Iron/Ferritin: Deficiency is common and can cause maternal anemia, which affects fetal growth.
- Folate and Vitamin B12: Both are vital for neural tube formation and healthy red blood cell production in the baby.
- Vitamin D and Calcium: Crucial for building strong bones in the developing fetus and maintaining the mother’s bone health.
If deficiencies are detected, targeted supplementation should start immediately to replenish nutrient stores before conception.
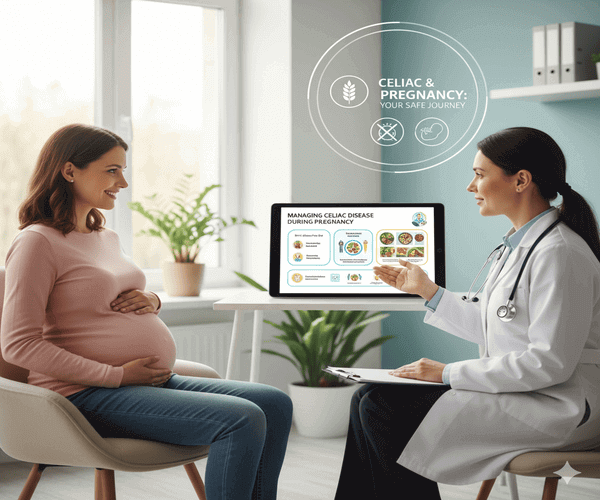
Assembling Your Healthcare Team
A successful journey through celiac disease and pregnancy requires a collaborative team. Ensure your team includes:
- Obstetrician-Gynecologist (OBGYN): Your primary prenatal care provider.
- Gastroenterologist: To monitor your Celiac status and serology.
- Celiac-Specializing Registered Dietitian (RD): To tailor your GFD to meet the heightened nutritional demands of pregnancy.
Managing Celiac Disease While Pregnant
Strict Gluten-Free Diet
The foundation of managing celiac disease and pregnancy is a gluten-free diet. Women should avoid wheat, rye, and barley. Safer alternatives include quinoa, rice, corn, buckwheat, and gluten-free oats.
Essential Nutrients to Focus On
During pregnancy, women with celiac disease should focus on:
- Iron: to prevent anemia.
- Folate: to reduce neural tube defects.
- Calcium and vitamin D: to promote bone health.
- Vitamin B12: for nervous system development.
Working with a Dietitian
A dietitian can help create balanced gluten-free meal plans, ensuring women meet nutritional needs during pregnancy.
Tips for dealing with Celiac Disease and pregnancy
- Stick to a strict gluten-free diet.
- Double-check food labels for hidden gluten.
- Avoid cross-contamination in cooking spaces.
- Keep a symptom and food journal.
- Visit both a gastroenterologist and an OB/GYN regularly.
FAQs About Celiac Disease and Pregnancy
Can celiac disease cause problems during pregnancy?
Yes. Untreated coeliac disease can elevate risks, including miscarriage and poor birth weight. With appropriate treatment, the majority of women experience healthy pregnancies.
Is a gluten-free diet safe during pregnancy?
Yes. A gluten-free diet is safe and essential when managing celiac disease and pregnancy. It prevents nutrient loss and supports fetal growth.
Will my baby inherit celiac disease if I have it?
Not necessarily. Having celiac disease increases the risk, but not all children will develop the condition. Monitoring by a pediatrician is recommended.
Can celiac disease affect fertility in women?
Yes, Fertility issues are sometimes linked to untreated celiac disease. Once the condition is managed with a gluten-free diet, fertility often improves.
What nutrients should pregnant women with celiac disease focus on?
Women should focus on iron, folate, calcium, vitamin D, and B12 to prevent deficiencies. Supplements may be required.
Can untreated celiac disease increase the risk of miscarriage?
Yes. Poor nutrient absorption in untreated celiac disease may raise miscarriage risks. A strict gluten-free diet lowers these chances.
How can I manage celiac disease effectively during pregnancy?
The best way to manage celiac disease and pregnancy is to stay gluten-free, avoid cross-contamination, take the right supplements, and follow up with healthcare providers.
Conclusion
The relationship between celiac disease and pregnancy is complex but manageable. With proper diagnosis, strict adherence to a gluten-free diet, and regular medical care, women with celiac disease can enjoy safe pregnancies and deliver healthy babies.
By understanding the risks and following best practices, expectant mothers can reduce complications and give their children the best possible start in life.
You must be logged in to post a comment.